- Applications
- پزشکی
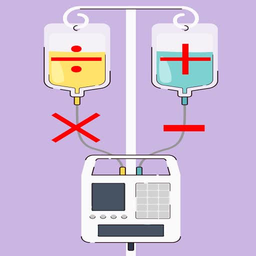
سرعت انفوزیون و محاسبات دارویی
| نصب | +۱ هزار |
| From ۲۴ Rates | 5 |
| Category | پزشکی |
| Size | ۲ مگابایت |
| Last Update | ۳۱ اردیبهشت ۱۴۰۲ |

| نصب | +۱ هزار |
| From ۲۴ Rates | 5 |
| Category | پزشکی |
| Size | ۲ مگابایت |
| Last Update | ۳۱ اردیبهشت ۱۴۰۲ |
Images








Introduction
زیربنای این نرم افزار که با راهنمایی خواهرزاده ام امیرمهدی شاهمیری به منظور اجرا بر روی تلفن همراه ساخته شده، بر اساس فرمولِ جامعی طراحی شده که توسط اینجانب محمدرضا سلطانی زرندی جهت محاسبه سرعت انفوزیون داروهای رقیق شده با محلول های انفوزیونی، ابداع شده است. نتایج پژوهش حاصل از ابداع فرمول فوق تحت عنوان
A Comprehensive Formula for Calculating the Infusion Rate of Medications Diluted with Infusion Solution
در ژورنال الکترونیکی
The Open Nursing Journal (ایندکس شده در Scopus)
به چاپ رسیده است.
به منظور بهبود نرم افزار به مرور موارد و منوهای جدیدی در زمینه محاسبات دارویی نیز به آن اضافه شده و خواهد شد:
منوهای نرم افزار:
1. محاسبه سرعت انفوزیون برای محلول های دارویی با زمان نامعین (مثال: محاسبه سرعت انفوزیون 2mcg/kg/min از محلول 200mg دوپامین حل شده در 100cc میکروست برای یک بیمار با وزن 70kg)
2. محاسبه سرعت انفوزیون برای محلول های دارویی با زمان معین (مثال: انفوزیون 2000cc سرم NS طی 24h)
3. محاسبه دوز داروهای درصدی (مثال : تعیین میزان دوز 100cc از محلول 7.5% بیکربنات سدیم)
4. محاسبه غلظت محلول ها (مثال: تعیین غلظت محلول حاصل از 10mg از یک دارو در 250cc سرم)
5. محاسبات اکی والان (تبدیل به سی سی و بالعکس) داروهای مهم
روش استفاده از نرم افزار:
الف: محاسبه سرعت انفوزیون محلول های دارویی بدون زمان معین:
ب: محاسبه سرعت انفوزیون محلول های دارویی با زمان معین:
همانطور که در قسمت 1 گفته شد، اگر مدت زمان کلی انفوزیون مشخص باشد (مثلاً 1000cc/24h)، شما باید از لیست اصلی، گزینه " محاسبه سرعت انفوزیون محلول های دارویی با زمان معین " را انتخاب کنید که در این صورت به صفحه دیگری هدایت می شوید که تنها باید در گزینه 1، حجم محلول (به سی سی)، در گزینه 2، ساعت انفوزیون (بر حسب ساعت) و در گزینه 3، نوع وسیله مورد استفاده جهت انفوزیون را انتخاب کنید . حال با کلیک بر روی "محاسبه سرعت انفوزیون " می توانید سرعت انفوزیون را بر حسب gtt/min و cc/h و همچنین فاصله قطرات بر حسب ثانیه را مشاهده کنید. (نکته: در صورت انتخاب گزینه میکروست، در سرعت نهایی محاسبه شده توسط نرم افزار، cc/h با gtt/min برابر است چرا که هر cc در میکروست، برابر با 60gtt می باشد؛ اگر ست سرم (با فاکتور 20gtt/cc) را انتخاب کرده باشید، عدد مربوط به gtt/min یک سوم برابر cc/h و اگر ست خون (با فاکتور 15gtt/cc ) را انتخاب کرده باشید، عدد مربوط به gtt/min یک چهار برابر cc/h خواهد بود. بدیهی است در صورتی که سرنگ را انتخاب کرده باشید، سرعت نهایی فقط بر حسب cc/h است و سرعت بر حسب cc/h و فاصله قطرات بر حسب ثانیه را نیز مشاهده نخواهید کرد).
ج: محاسبه داروهای درصدی:
1. در گزینه 1، نوع تبدیل را انتخاب کنید (تبدیل حجم به جرم / جرم به حجم).
2. با انتخاب گزینه "تبدیل حجم به جرم" و وارد کردن حجم دارو به cc (در گزینه 2) و درصد دارو (در گزینه 3) و کلیک بر روی "محاسبه" میتوانید میزان داروی مورد نظر را به mg و gمشاهده کنید.
3. با انتخاب گزینه "تبدیل جرم به حجم " و وارد کردن جرم دارو به mg (در گزینه 2) و درصد دارو (در گزینه 3) و کلیک بر روی "محاسبه"، میتوانید میزان داروی مورد نظر را به cc مشاهده کنید. دقت داشته باشید که اگر جرم داروی مورد نظر شما بر حسب g باشد باید آن را در 1000 ضرب نمایید و سپس آن را وارد نمایید. (1gr=1000mg)
د: تعیین غلظت محلول های دارویی:
با انتخاب این گزینه و وارد کردن میزان داروی رقیق شده و انتخاب واحد آن (به mg و g) و سپس وارد کردن حجم محلول به سی سی، میتوانید غلظت محلول دارویی را مشاهده کنید. بدیهی است در صورت انتخاب واحد mg، غلظت محلول دارویی بر حسب mcg/ml و در صورت انتخاب واحد g، غلظت محلول دارویی بر حسب mg/mlخواهد بود.
و: محاسبات اکی والان:
1. در گزینه 1، نوع تبدیل را انتخاب کنید (تبدیل سی سی به میلی اکی والان / میلی اکی والان به سی سی).
2. با انتخاب "سی سی به میلی اکی والان" (در گزینه 1)، انتخاب نام دارو (در گزینه 2)، وارد کردن حجم دارو به cc (در گزینه 3) و کلیک بر روی "محاسبه"، میتوانید میزان داروی مورد نظر را به mEq(میلی اکی والان) مشاهده کنید.
3. با انتخاب " میلی اکی والان به سی سی " (در گزینه 1)، انتخاب نام دارو (در گزینه 2)، وارد کردن میزان دارو به mEq (میلی اکی والان) (در گزینه 3) و کلیک بر روی "محاسبه"، میتوانید میزان داروی مورد نظر را به ccمشاهده کنید.
ه. رقیق سازی و کاهش درصد دارو:
1. در گزینه 1، درصد داروی فعلی را انتخاب کنید (مثلاً اگر میخواهید بی کربنات 8.4% را به 7.5% تبدیل کنید، در اینجا عدد 8.4را وارد کنید).
2. در گزینه 2، درصد داروی رقیق شده نهایی را وارد کنید (مثلاً اگر میخواهید بی کربنات 8.4% را به 7.5% تبدیل کنید، در اینجا عدد 7.5را وارد کنید).
3. در گزینه 3، حجم داروی رقیق رقیق شده نهایی را وارد کنید (مثلاً اگر میخواهید با رقیق کردن بی کربنات 8.4%، میزان 10cc بی کربنات 7.5% به دست آورید، در اینجا عدد 10را وارد کنید).
4. با کلیک بر روی "محاسبه حجم برداشتی از داروی فعلی جهت رقیق سازی"، می توانید حجم مورد نیاز را به cc به دست آورید. (مثلاً اگر میخواهید با رقیق کردن بی کربنات 8.4%، میزان 10cc بی کربنات 7.5% به دست آورید، در اینجا عدد 8.92 را مشاهده خواهید کرد که اگر این میزان از بی کربنات 8.4% را تا میزان 10cc رقیق کنید، درصد داروی نهایی 7.5%خواهد بود).
ی: غلیظ سازی و افزایش غلظت دارو / سرم:
1. در گزینه 1، درصد داروی رقیق تر موجود را انتخاب کنید (مثلاً اگر میخواهید NaCl0.45% را با کمک NaCl5% به NaCl0.9% با حجم 1000ccتبدیل کنید، در اینجا عدد 0.45 را وارد کنید).
2. در گزینه 2، درصد داروی غلیظ تر موجود را وارد کنید (در مورد مثال فوق، در اینجا عدد 5را وارد کنید).
3. در گزینه 3، درصد داروی مورد نیاز را وارد کنید (در مورد مثال فوق، در اینجا عدد 0.9 را وارد کنید).
4. در گزینه 4، حجم محلول مورد نیاز را وارد کنید (در مورد مثال فوق، در اینجا عدد 1000را وارد کنید).
5. با کلیک بر روی "محاسبه حجم برداشتی از داروی فعلی جهت غلیظ سازی"، می توانید حجم مورد نیاز از محلول رقیق تر و غلیظ تر موجود را به cc به دست آورید. (در مورد مثال فوق، در اینجا V1 میزان لازم از محلول 0.45% و V2 میزان لازم از محلول 5% را نشان خواهد داد که باید با هم مخلوط شوند تا 1000cc محلول NaCl0.9%تهیه شود).
استفاده از این نرم افزار را به تمامی پزشکان، پرستاران، ماماها، کارشناسان بیهوشی، کارشناسان اتاق عمل و سایر کارکنان عزیز و بزرگوار کادر درمان درگیر در دارودهی به بیماران توصیه می نماییم.
--------------------------------------------------------------------------------------------------------------------
سوابق به روز رسانی نرم افزار:
1402/02/20:
اضافه شدن گزینه «غلیظ سازی و افزایش غلظت محلولهای دارویی»
1402/02/16:
اضافه شدن گزینه «رقیق سازی و کاهش غلظت محلولهای دارویی»
01/02/1402:
1. باز طراحی کامل نرم افزار جهت سهولت استفاده (ظاهر)
2. ادغام گزینه های تبدیل میلی اکی والان به سی سی و بالعکس جهت دسترسی سریعتر
3. اضافه شدن گزینه "تبدیل جرم به حجم" به منوی محاسبه داروهای درصدی
26/01/1400:
اضافه شدن گزینه محاسبات مربوط به اکی والان (تبدیل میلی اکی والان به سی سی و بالعکس)
01/11/1399:
اضافه شدن گزینه محاسبه غلظت محلول دارویی
28/10/1399:
1. اضافه شدن گزینه فاصله قطرات
2. اضافه شدن منوهای کشویی
3. اضافه شدن گزینه محاسبه داروهای درصدی (حجم به جرم)
4. اضافه شدن منوی روش استفاده از نرم افزار
23/09/1399:
1. اضافه و مجزا نمودن دو پاسخ سی سی بر ساعت و قطره بر دقیقه برای ست های مختلف جهت استفاده هم برای پمپ انفوزیون (قطره بر دقیقه ) و هم پمپ سرنگ (سی سی بر ساعت) در مورد تمامی دستورات پزشک
2. اضافه نمودن معادل فارسی در مورد تمامی دستورات پزشک
3. اضافه نمودن فاکتور قطره (تعداد قطره به ازاء هر سی سی) برای تمامی وسایل مورد استفاده جهت آنفوزیون
4. اضافه نمودن نام و لینک سایر کتابهای نرم افزاری محمدرضا سلطانی زرندی در بازار
12/09/1399:
1.اضافه شدن محاسبه سرعت آنفوزیون سرم ها و محلول های با زمان معین
۲. اضافه شدن گزینه نظر دهی در بازار
02/09/1399 : انتشار اولیه نرم افزار به صورت محاسبه سرعت انفوزیون محلول های بدون زمان معین



برنامههای مرتبط










دیگران نصب کردهاند


















